Shabbar F. Danish, MD, FAANS (left)
Shabbar F. Danish, MD, FAANS (left)
Chief, Section of Neurosurgical Oncology, /
New Brunswick, New Jersey
Brian V. Nahed, MD, MSC (middle)
Assistant Professor of Neurosurgery, /
Boston, MA
Nitesh V. Patel, MD (right)
Neurosurgery Resident,
New Brunswick, New Jersey
More than 70,000 patients will learn that they have a new primary brain tumor this coming year in the United States alone.6 While most of these patients will undergo surgery for removal and diagnosis, there are some for whom surgery is not a good option.5 Historically, treatment interventions for these individuals were more limited. Neurosurgeons frustrated by this limitation have been involved in the development and study of two new FDA-approved treatments. These are thermal therapy systems that sparked a renewed interest in Magnetic Resonance Guided Laser Induced Thermal Therapy (MRgLITT). LITT provides a minimally invasive surgical access coupled with the power of lasers to ablate a tumor from the inside out.
MRgLITT is performed using a navigation system which specifically targets a point in the brain using three-dimensional coordinates called stereotaxis.4 The procedure is simple:
- A small incision is made in the skin;
- A small hole in then created in the skull;
- The laser catheter is placed into the tumor in the brain;
- Location of the laser is confirmed by live MR thermometry; and
- Tumor tissue is ablated using real-time MRI.
Imagine, the signals (called pixels) on the MRI images change as the tissue is ablated! This allows real-time tracking to determine the extent of tumor destruction. Temperature limits are set within and around the target to reduce the chance of damage to surrounding healthy tissue.
MRgLITT has been demonstrated to be efficacious in a variety of brain lesions including:
- Primary brain tumors (gliomas);
- Tumors that spread to the brain (metastatic lesions); and
- Radiation necrosis.1
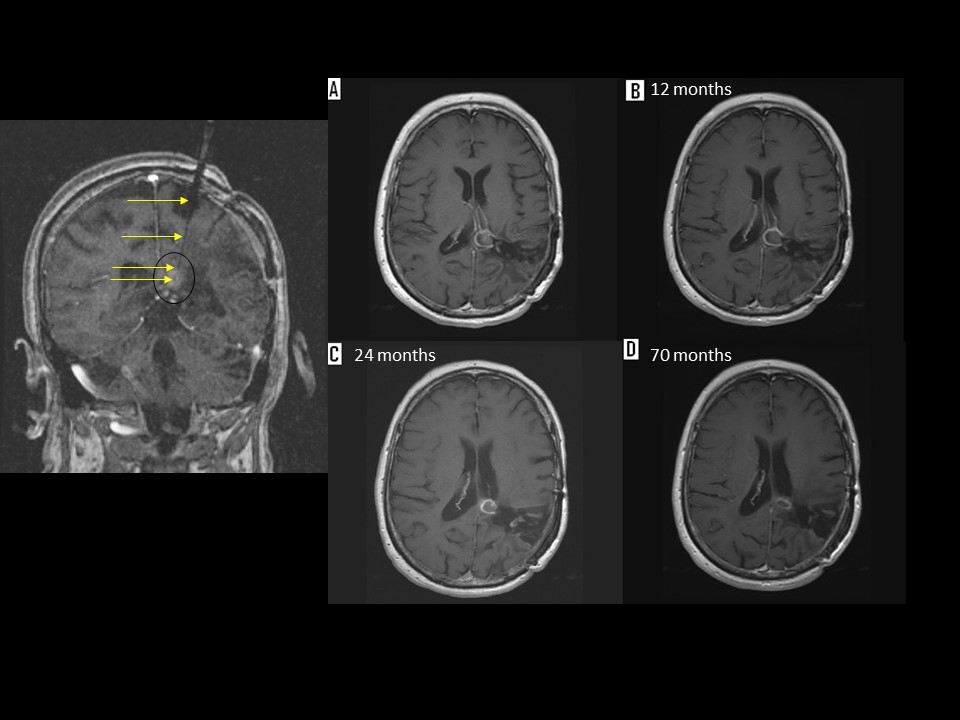
Figure: This is a patient with a recurrent anaplastic ependymoma located below the splenium of the corpus callosum. The patient had undergone multiple craniotomies, fractionated radiation as well as radiosurgery. She underwent placement of a transparietal laser catheter using the Visualase System (Left image). The images on the right represent the follow up images after MRI guided laser therapy.
For those patients who cannot undergo surgery for any number of reasons, MRgLITT may provide a novel therapeutic option.5 Prior treatment strategies, such as radiation, are limited by dose constraints, and chemotherapy is limited by tumor resistance and getting the agent into the brain (due to blood-brain barrier impermeability).2,3 Real-time monitoring of ablation allows for immediate and direct control of therapy, which can be modified during the intervention in real-time. After surgery, the laser catheter is easily removed, and the skin closed with a stitch. Patients typically spend just 24 hours in the hospital after the procedure before discharge. The treatment is safe with few complications that require the patient return to the hospital (data show less than 6 percent of patients had complications leading to readmission at 30 days after MRgLITT).7
MRgLITT is a promising option that offers hope, but there are still some challenges that require further work:
- Swelling may get worse after treatment which may cause the patient to develop neurological issues.
- The natural shape of most tumors is irregular while the laser heat distribution follows a spherical fashion. Modification of the procedure such as stepwise treatment or use of multiple catheters may allow the laser to cover more volume.
- Fluids in the brain such as ventricles and blood vessels may alter the effect of the laser by creating a heat sink effect and lead to asymmetric heat distribution.
Neurosurgeons will continue to work to overcome these difficulties to bring innovative, minimally invasive new treatment to our many patients who are found to have brain tumors. MRgLITT provides an innovative tool in the neurosurgical armamentarium, especially for previously inaccessible surgical lesions.
References:
- Attaar SJ, Patel NV, Hargreaves E, Keller IA, Danish SF: Accuracy of Laser Placement With Frameless Stereotaxy in Magnetic Resonance-Guided Laser-Induced Thermal Therapy. Neurosurgery:14, 2015
- Henson JW, Cordon-Cardo C, Posner JB: P-glycoprotein expression in brain tumors. J 14:37-43., 1992
- Idbaih A, Omuro A, Ducray F, Hoang-Xuan K: Molecular genetic markers as predictors of response to chemotherapy in gliomas. Curr Opin Oncol. 19:606-611., 2007
- Jethwa PR, Barrese JC, Gowda A, Shetty A, Danish SF: Magnetic resonance thermometry-guided laser-induced thermal therapy for intracranial neoplasms: initial experience. 71:133-144; 144-135. doi: 110.1227/NEU.1220b1013e31826101d31826104., 2012
- Medvid R, Ruiz A, Komotar RJ, Jagid JR, Ivan ME, Quencer RM, et al: Current Applications of MRI-Guided Laser Interstitial Thermal Therapy in the Treatment of Brain Neoplasms and Epilepsy: A Radiologic and Neurosurgical Overview. AJNR Am J Neuroradiol. 36:1998-2006. doi: 1910.3174/ajnr.A4362. Epub 2015 Jun 1925., 2015
- Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al: CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008-2012. Neuro Oncol. 17:iv1-iv62. doi: 10.1093/neuonc/nov1189. Epub 2015 Oct 1027., 2015
- Purvee Patel B, Nitesh V Patel, MD, Shabbar F. Danish, MD: Intracranial Magnetic Resonance Guided Laser Induced Thermal Therapy (MRgLITT): Single Center Experience with the Visualase Thermal Therapy System Journal of Neurosurgery In Production / Press, 2015